Concussion in the ED: New Guidelines and Accurate Diagnoses
Submitted by: Ernest Wang, MD,
with Nicole Reams, MD,
NorthShore University HealthSystem
It may come as no surprise, given our experiences each day in Emergency Departments (ED) across the country, that the most recent data from the CDC reports visits to the ED due to traumatic brain injury (TBI) have increased by more than 50% between 2007-20131, and the numbers continue to rise.
Even further:
- Emergency department visits for brain injuries among adults age 65+ more than doubled; hospitalizations and deaths increased by more than 30 percent.
- Nearly a third (29.9 %) of all concussions were sports-related, and of those, over two-thirds (70%) of concussions among high school athletes result from colliding with another athlete.
Last year, the CDC released new guidelines on diagnosing and managing children with concussion2, recognizing the increase in injuries and the lack of consistency in treatment and management. Given this remarkable increase in ED visits for TBI and concussion, I recently spoke with Nicole Reams, MD, Section Head for the Department of Neurology’s Concussion Program at NorthShore University HealthSystem, to discuss details of the new guidelines for concussion care, and to identify signs and symptoms that may mask an accurate concussion diagnosis.
Q: In the Emergency Department, the most common type of concussion cases we see are patients who have fallen, and hit their heads. We can recognize those patients who immediately need a CT scan (i.e., significant loss of consciousness, amnesia, confusion, seizure, focal neurologic deficits, external signs of trauma), but what about those that are more subtle? Often times patients come in a day or two after the injury, due to continued symptoms. They may not have lost consciousness but feel dizzy or nauseous. Do we need to be aware of other symptoms or signs of concussed patients that may be overlooked?
A: Certainly the red flag signs of brain injury are those you highlighted: progressive decline in cognition or awareness, new focal signs like weakness or numbness, recurrent vomiting, asymmetric pupils, or significantly worsening course over time.
Most patients with concussion will not have these symptoms and will experience a varied presentation from patient to patient of headaches, dizziness, imbalance, photophobia, phonophobia, cognitive change (ranging from disorientation to subtle “fogginess” or trouble with concentration), nausea with or without vomiting, sleep and/or mood dysfunction. Some individuals experience all of these symptoms and some present with just a few. The most helpful parts of the examination are cervical range of motion, high cervical palpation (to see if there is additional cervical strain contributing to headaches), eye movement testing to look for conjugate movements, nystagmus, saccades, convergence, and vestibulo-ocular reflex, as well as patient tolerance of these maneuvers, and lastly, balance: I typically test Romberg, tandem gait, and single leg stance.
Q: One of the biggest challenges we as emergency physicians face with concussed patients is deciding whether or not to perform a CT scan in both adults and children. The American College of Emergency Physicians, as part of the Choosing Wisely initiative, has disseminated a Clinical Policy on neuroimaging and decision making in adult mild traumatic brain injury in the acute setting. In addition validated decision rules such as PECARN can assist with avoidance of CT scans of the head in low risk pediatric patients who present less than 24 hours after the event. Are there any red flags in patients who present in delayed fashion with non-focal concussive symptoms as you describe above that increase their risk of a significant bleed? Should they be imaged? If so, which modality is preferred?
A: There are no validated guidelines for signs or symptoms of delayed bleed. My advice would be that if a patient is presenting with a significantly worsening or altered course (sudden change in severity of headaches, new lethargy) or new focal neurologic signs, that imaging should be done. CT remains the imaging tool of choice to screen for bleed, even when delayed by a few days.
Q: When a child comes into the ED with potential concussion, our first concern is to make sure they don’t have a significant head injury. But once they leave our care, my concern is that they receive appropriate follow-up to be evaluated for any residual effects. What are your recommendations on protocol for follow-up care for pediatric patients?
A: There are no published guidelines regarding timing of follow-up for pediatric patients but my recommendation is that pediatric patients with suspected or confirmed concussion be seen by either their primary care physician or the concussion clinic (by a specialist with expertise in concussion, typically a neurologist) within 2-3 days of discharge from the ED. Concussion is an evolving injury and symptoms can change in this short time window for many individuals so expedited follow-up is important.
Q: Once patients are diagnosed with concussion, they have many questions about the after care and necessary precautions (especially given recent news and updates on guidelines, as covered by mainstream media.) Conflicting information can be confusing, especially after they conduct a quick Google search while they are in my care. Can you please clarify the guidelines for adult post-concussion care, including resources or sites you find valuable to direct patients?
A: Early concussion management is relative rest, which means scaling down one’s activity from normal, taking breaks as needed, and avoidance of intense physical exertion. In regards to cognitive exertion (homework, reading, screen time) and light physical exertion (household chores, walking the dog, going up the stairs), patients are encouraged to do these activities from the very beginning of the injury, but to do so in short increments (i.e. 10 minutes at first) and take a break so as not to exacerbate symptoms. The patient is likely to tolerate longer time intervals over time and he should increase cognitive exertion as tolerated. Once the patient can tolerate at least one normal day of school or work without symptoms (24+ hours), then beginning a gradual return to physical exercise can be considered.
Q: The American Academy of Pediatrics recently updated their guidelines on returning to activities post-concussion. Can you give us some details on those updates, and what we need to share with our patients?
A: The American Academy of Pediatrics (AAP) recently published new guidelines for Sport-Related Concussion in Adolescents in Children in December 2018 as an update to guidelines they published in 2010. In this article, they review scientific evidence regarding the pathophysiology, epidemiology, signs and symptoms, acute assessment, neuroimaging, neurocognitive testing, acute management, return to play, prolonged symptoms, potential long-term effects, and prevention of concussion. The most notable updates come in the area of the acute post-concussion management. The previous clinical report emphasized the role of cognitive rest. More recent research has revealed that there may be negative consequences from strict rest resulting in increased symptom burden and longer recovery times. In light of this, the AAP is still recommending removal from play following concussion, but recommending avoiding complete inactivity. Light cardiovascular activity which is subsymptom threshold can be beneficial. AAP also endorsed returning to school with academic accommodations but avoiding prolonged school absence as well as continued use of electronics and social media with adjustments or breaks as needed. 5
Q: Is there anything else you’d like us to consider when caring for concussion patients in the ED, to better improve their outcomes once they see their neurologist for follow-up care?
A: Patients with severe symptoms, atypical presenting symptoms, complicated past medical history that may predispose to prolonged recovery (ie migraine, ADHD, depression or anxiety), prolonged loss of consciousness (>1 minute), seizure at impact, history of multiple concussions, or those returning to athletics should be considered more specifically for referral to a specialty concussion clinic for assessment and treatment by a neurologist with expertise in concussion, if your institution has one available. Also keep in mind that although most concussions are self-limiting injuries and resolve quickly, some individuals have an extended course with concussion recovery and there may be patients that present to the ED with multiple neurologic symptoms such as headaches, dizziness, nausea, and confusion several weeks or even months after a head injury, so it may be prudent to search for a history of head injury and ensure there is proper work-up and referral follow-up for this potential diagnosis.
Ernest Wang, MD, FACEP
ICEP President-Elect
Nicole Reams, MD
Section Head, Concussion Program, Department of Neurology, NorthShore University HealthSystem, Evanston
Additional Resources:
Video instructions for eye movement testing if interested:
https://www.youtube.com/watch?v=XlA_wJAMBmg
https://m.youtube.com/watch?v=CJF6kJcFGqE
3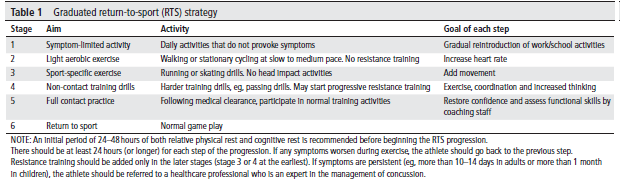
4 CDC.Gov has great resources for concussion information. Start here: https://www.cdc.gov/headsup/basics/index.html
Authors
Dr. Ernest Wang is the Alvin H. Baum Family Fund Chair of Simulation and Innovation, Assistant Dean for Medical Education, and Associate Chief for the Division of Emergency Medicine at NorthShore University HealthSystem in Evanston, IL. He is a Clinical Professor of Emergency Medicine at the University of Chicago Pritzker School of Medicine. He is the President-Elect for ICEP.
Dr. Nicole Reams is the Section Head for the Department of Neurology’s Concussion Program at NorthShore University HealthSystem. She one of the country’s few fellowship-trained Sports Neurologists. She serves as the medical chair for United States Intercollegiate Boxing Association where she also serves as a ringside physician. Dr. Reams is the independent neurologic consultant and an unaffiliated neurotrauma consultant for the Chicago Bears and the independent neurologic consultant for Northwestern University Athletics. She also is a consultant for the Chicago Blackhawks, Chicago Fire, and Chicago Lions. She serves on several local and national committees for concussion policy and education.
References
- Traumatic Brain Injury in the United States. https://www.cdc.gov/traumaticbraininjury/pdf/TBIInTheUnitedStates-PublicHealthProfessionals.pdf
- CDC Pediatric mTBI Guideline.https://www.cdc.gov/traumaticbraininjury/PediatricmTBIGuideline.html
- McCrory P, Meeuwisse W, Dvorak J, et al. Br J Sports Med. 2018; 51:838–847.
- Brain Injury Basics. https://www.cdc.gov/headsup/basics/index.html Accessed December 21, 2018.
- Halstead ME, Walter KD, Moffatt K. Sport-Related Concussion in Children and Adolescents. Pediatrics. 2018; 142(6):e20183074.
- Kuppermann N, Holmes JF, Dayan PS, et al. Pediatric Emergency Care Applied Research Network (PECARN). Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009 Oct 3;374(9696):1160-70. Epub 2009 Sep 14. Erratum in Lancet 2014 Jan 25;383(9914):308.
- Jagoda AS, Bazarian JJ, Bruns JJ Jr, Cantrill SV, Gean AD, Howard PK, Ghajar J, Riggio S, Wright DW, Wears RL, Bakshy A, Burgess P, Wald MM, Whitson RR; American College of Emergency Physicians; Centers for Disease Control and Prevention. Clinical policy: neuroimaging and decisionmaking in adult mild traumatic brain injury in the acute setting. Ann Emerg Med. 2008 Dec;52(6):714-48.
- Avoid computed tomography (CT) scans of the head in emergency department patients with minor head injury who are at low risk based on validated decision rules. http://www.choosingwisely.org/clinician-lists/american-college-emergency-physicians-ct-scans-of-head-for-emergency-department-patients-with-minor-head-injury/